Deep peroneal nerve block
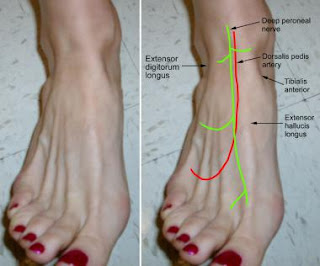
In the leg, the deep peroneal nerve supplies muscular branches to the tibialis anterior, extensor digitorum longus, peroneus tertius, and extensor hallucis longus. It also provides an articular branch to the ankle joint. Two cm distal to the intermalleolar line, the following structures (from medial to lateral) are related to the deep peroneal nerve:
- Tendon of tibialis anterior
- Tendon of extensor hallucis longus
- Dorsal pedis artery
- Deep peroneal nerve
- Tendon of extensor digitorum longus
Blocking the following five nerves (3 superficial and 2 deep) results in complete block of sensory perception beneath the ankle:
- Superficial peroneal nerve
- Saphenous nerve
- Sural nerve
- Deep peroneal nerve
- Posterior tibial nerve
All 5 nerves should be blocked if a tourniquet is used for foot surgery.[4]
Indications
- Surgeries involving the first web space of the foot (eg, Morton neuroma)
- Component of ankle block (Ankle block is preferred for foot surgeries in patients who may not tolerate epidural or spinal anesthetic.)
- Treatment of acute or chronic pain conditions involving the foot with entrapment of the deep peroneal nerve at the anterior tarsal tunnel (Anterior tarsal tunnel syndrome is characterized by persistent aching of the dorsum of the foot that is worse at night and is made better by moving the affected toes and ankle. Sometimes, patients experience weakness of toe extensors. Patients with diabetes may be more prone to this condition. It can occur after prolonged squatting or leaning forward.)
- As a palliative measure and a part of multimodal approach to pain management of acute pain from foot fracture or gouty arthritis
- As a prelude to neurolysis or radiofrequency ablation of the deep peroneal nerve.
Contraindications
- Patient refusal
- Infection at the injection site
- Coagulopathy
Anesthesia
- Infiltrate area of skin for nerve block with 0.5-1 mL of lidocaine 1%.
- For more information, see Local Anesthetic Agents, Infiltrative Administration.
Equipment
- Alcohol, povidone-iodine (eg, Betadine), or chlorhexidine (Hibiclens) preparatory solution.
- Syringe, 5 mL, 25-27 gauge 1-inch needle
- Anesthetic, 5 mL (lidocaine 1%, bupivacaine 0.5%, or ropivacaine 0.5%)
- Depot corticosteroid (eg, methylprednisolone acetate [Depo-Medrol] 40 mg, triamcinolone acetonide [Kenalog] 40 mg)
- Gauze, 2 X 2
- Sterile gloves
- All resuscitative equipment
- Standard monitors
- Adhesive bandage
Positioning
See the list below:
- Position the patient supine with the toes dorsiflexed to identify the tibialis anterior, extensor hallucis longus, and extensor digitorum longus tendons.
Technique
The deep peroneal nerve is traditionally located by identifying the surface landmarks, shown below. Other methods of identifying the injection site include invoking paresthesia, using a nerve stimulator, and ultrasonographic guidance.[5, 6]
Perimalleolar approach
- Perform a careful neurological assessment prior to the procedure.
- Identify the tendon of extensor hallucis longus by big toe dorsiflexion against resistance. A groove is felt just lateral to the tendon.
- The deep peroneal nerve lies lateral to the tendon and the dorsalis pedis artery. Lateral to the nerve is the tendon of the extensor digitorum longus. The needle entry site is about 2 cm distal to the intermalleolar line, just lateral to the dorsalis pedis artery pulse.
- After the skin is prepared, raise a skin wheal with the 0.5-1 mL of the local anesthetic.
- Next, advance the same needle and syringe that contains the local anesthetic through the skin in a perpendicular manner until bone is encountered, usually within 2-3 cm.
- Withdraw the needle slightly to prevent periosteal injection.
- Patients may experience paresthesia in the first web space. If paresthesia occurs, withdraw the needle slightly until the paresthesia disappears.
- After careful negative aspiration for heme, inject 2 mL of the local anesthetic.
- To increase the block success, the needle may be redirected 30º medially and laterally and an additional 2 mL of the anesthetic injected.
- Remove the needle and apply firm pressure to prevent bleeding.
- If the condition has an inflammatory component, methylprednisolone 40 mg or triamcinolone 40 mg may be added to the injectate.
- If a nerve stimulator is used (2-3 mA at 0.1 ms), extension of the lateral 4 toes due to muscle twitch of the extensor digitorum brevis may be used to locate the nerve. [7]
Inframalleolar or midtarsal approach
- Insert the needle immediately lateral to the extensor hallucis longus tendon but medial to the dorsalis pedis artery.
- After negative aspiration, inject 5 mL of local anesthetic as described above. [8, 9, 10]
Pearls
See the list below:
- The deep peroneal nerve is one of the 2 deep nerves at the ankle. The deep peroneal nerve may be blocked as a part of a total ankle block.
- The deep peroneal nerve innervates the first web space.
- At the malleolar level, the deep peroneal nerve is located between the tendons of extensor hallucis longus and extensor digitorum longus, in close proximity to the dorsalis pedis artery.
- To increase the block success, redirect the needle 30º and inject additional local anesthetic after the initial injection.
- Careful neurological assessment is important prior to the procedure; it helps avoid later attribution of preexisting neurological deficits to the nerve block.
Complications
The block is essentially safe block to perform, but some complications can occur.
- Intravascular injection: The dorsalis pedis artery should be carefully palpated to minimize the chance of intravascular injection of local anesthetic.
- Ecchymosis and hematoma: These complications can be avoided by applying firm pressure to the injection site after the injection.
- Paresthesia: To avoid needle-induced trauma to the nerve, withdraw the needle slightly before the injection.
No comments:
Post a Comment